Gastric Bypass: What to Expect and Key Benefits
If you have been navigating the complex world of weight management and traditional methods haven’t provided the sustainable change you need, you might be looking at bariatric surgery. This type of surgery isn’t just a quick fix; it’s a powerful tool designed to kickstart a total lifestyle transformation. Among the options available, the procedure known as gastric bypass remains one of the most recognized and effective methods globally.
Deciding to pursue gastric bypass is a monumental moment, full of hope, questions, and maybe a little anxiety. This surgery fundamentally changes how your body handles food, leading to significant and often rapid weight loss. We’re here to demystify the process, explain exactly how the surgery works, and address the crucial factors—like cost and recovery—so you can step into this journey with confidence and expertise.

How Does Roux-en-Y Gastric Bypass Surgery Work?
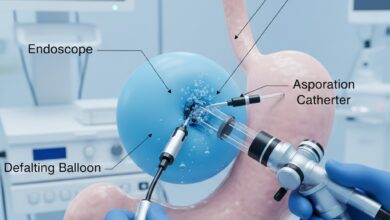
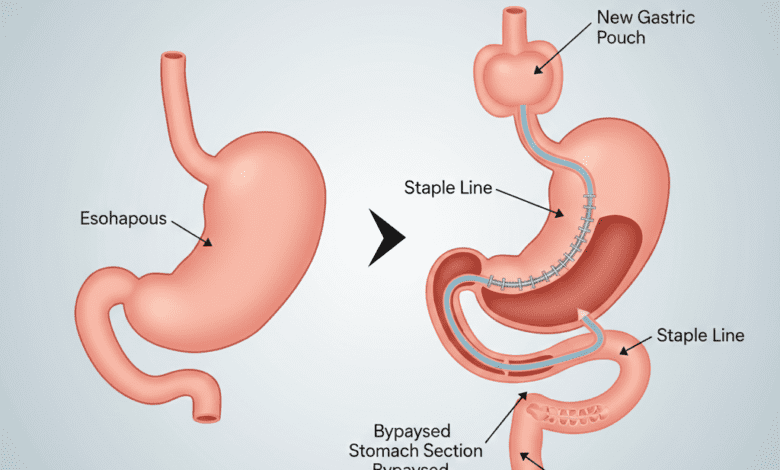
The gastric bypass surgery, specifically the Roux-en-Y technique, is considered the gold standard of bariatric procedures. It’s a complex operation that combines restriction (limiting how much food you can eat) and malabsorption (limiting how many calories your body can absorb). Understanding the mechanics of the Roux-en-Y procedure is key to grasping why it’s so effective for long-term weight management and metabolic health improvement.
The overall goal is twofold: reducing stomach capacity and altering the digestive pathway. This dual action is what sets it apart from simpler restrictive procedures.
The Small Pouch Creation
First, the surgeon uses staples to divide the stomach into two sections. They create a very small upper pouch, roughly the size of a walnut or a small egg. This tiny pouch is where food will land after you swallow. Because it holds only about an ounce of food, you feel full very quickly, drastically reducing calorie intake. The larger, bypassed portion of the stomach remains in the body but no longer receives or digests food.
Rerouting the Small Intestine (The “Roux Limb”)
Next comes the “bypass” part of the roux en y. The surgeon divides the small intestine and connects the newly created small stomach pouch directly to a lower segment of the intestine. This connection is called the Roux limb. This rerouting means that food now skips the majority of the stomach and the first section of the small intestine (the duodenum). By bypassing these areas, the body absorbs fewer calories and nutrients, leading to weight loss. Moreover, this rearrangement significantly changes gut hormone signals, which can help control appetite and improve conditions like Type 2 diabetes almost immediately after surgery.
Navigating the Recovery and Long-Term Commitment
While the surgery itself is usually performed minimally invasively (laparoscopically), the recovery period requires dedication. Most patients spend 2 to 3 days in the hospital. The first few weeks post-operation are strictly dedicated to healing and adjusting to the new diet, which progresses slowly from clear liquids to pureed foods, and eventually to solid foods.
Crucially, the success of a gastric bypass operation depends entirely on a lifelong commitment to dietary changes and regular exercise. Since nutrient absorption is reduced, patients must take lifelong vitamin and mineral supplements (like B12, iron, calcium, and Vitamin D) to prevent deficiencies. This ongoing medical management is non-negotiable for staying healthy after the procedure.
Understanding Gastric Bypass Surgery Cost and Coverage
When exploring the possibility of major metabolic surgery, one of the most pressing concerns for patients is the gastric bypass surgery cost. It’s important to understand that this is a significant investment in your health, and the price tag reflects the complex nature of the procedure, the hospital resources, and the specialized surgical team required.
Factors Influencing the Price Tag
The overall cost of the procedure can vary widely—typically ranging from $15,000 to over $35,000—based on several variables. These include the geographic location of the hospital, the experience level of the bariatric surgeon, and whether complications arise. The total fee usually covers pre-operative testing, the surgical procedure itself, anesthesia, hospital stay, and necessary follow-up care for the initial weeks.
Insurance and Financial Aid Options
While the sticker price might seem daunting, many patients do not pay the full amount out-of-pocket. Most insurance providers, including Medicare and Medicaid, offer coverage for gastric bypass if the patient meets specific medical criteria. Generally, this involves having a certain Body Mass Index (BMI) and documentation of failed attempts at physician-supervised weight loss.
If you are self-paying or your insurance denies coverage, many bariatric centers offer financing options or package pricing that bundles all necessary services. Always consult with the hospital’s financial coordinator early in the process to understand your coverage details and explore potential financial assistance programs. Thorough preparation regarding the financial aspects is a critical step in preparing for any gastric bypass procedure.
The gastric bypass is more than just a weight loss tool; it is a life-altering medical intervention that addresses metabolic health on a fundamental level. By utilizing the highly effective roux en y technique, patients gain the opportunity to resolve serious health conditions like Type 2 diabetes and hypertension, alongside achieving profound and sustainable weight loss. While the journey demands commitment—from adhering to post-operative diet restrictions to managing the financial planning—the potential for a longer, healthier, and more active life makes the gastric bypass a transformative choice for eligible individuals.