Deciding to pursue significant weight loss is one of the biggest and most personal decisions you can make. If you have spent years navigating diets, workout routines, and fluctuating results, you may have reached a point where you are researching surgical options. For millions of people seeking a permanent reset button for their health, the answer often lies in the procedure known as the gastric sleeve.
This procedure, technically called sleeve gastrectomy, has quickly become the most commonly performed weight-loss operation worldwide. Its popularity stems from its highly effective results coupled with a relatively straightforward recovery compared to older, more complex operations. The goal of the gastric sleeve is not just to help you lose weight, but to dramatically improve obesity-related health conditions, from type 2 diabetes to sleep apnea.
If you are exploring this option, you probably have dozens of questions about how it works, what it costs, and if you are a good candidate. Understanding the mechanism behind the gastric sleeve is the first step toward reclaiming your health and achieving long-term wellness goals.
Understanding Gastric Sleeve Surgery and How it Works
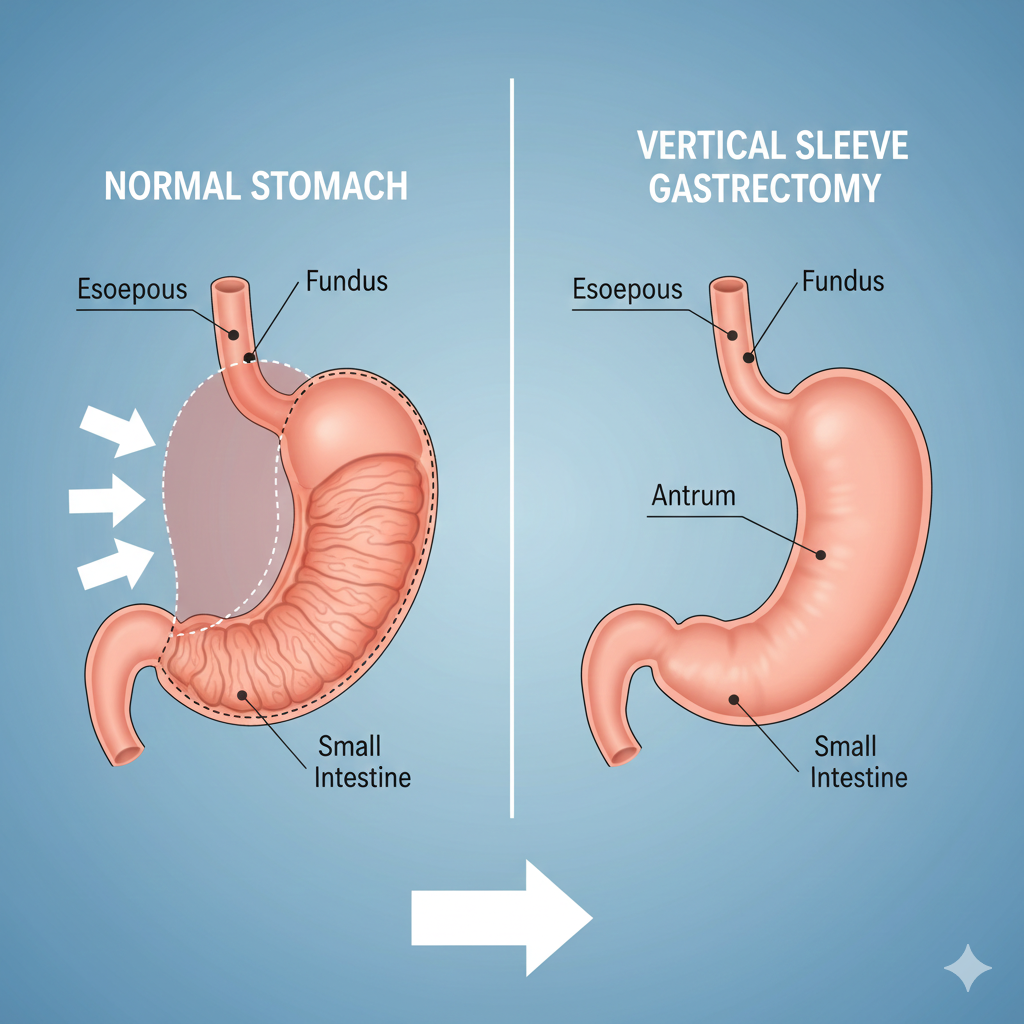
The official medical term for the procedure is vertical sleeve gastrectomy (VSG), but most people simply refer to it as gastric sleeve surgery. It is a surgical procedure, typically performed laparoscopically—meaning through several small incisions—that fundamentally changes the structure of your stomach. Unlike other older procedures that rerouted the small intestine, the sleeve focuses purely on restriction.
During the operation, surgeons permanently remove approximately 75 to 80 percent of the stomach. What remains is a narrow, tube-like structure, or “sleeve,” about the size and shape of a banana. This smaller stomach capacity limits the amount of food you can consume in one sitting, leading to significantly reduced calorie intake.
The effectiveness of this surgery is not just physical; it is hormonal. By removing the large outer curve of the stomach, the surgery also removes the primary production site of ghrelin, often referred to as the “hunger hormone.” Patients typically experience a marked reduction in appetite and cravings, making it easier to stick to a healthy, controlled eating plan post-operation.
The Difference Between Restrictive and Malabsorptive Procedures
It is important to understand that the gastric sleeve is a purely restrictive procedure. It limits the volume of food intake without altering the normal digestive process of nutrient absorption in the small intestine. This is a key difference from malabsorptive operations, such as gastric bypass, which reduce both volume and the body’s ability to absorb calories and nutrients. Because the gastric sleeve maintains normal absorption, the risk of serious long-term vitamin deficiencies is generally lower, though supplementation is always required.
Recovery Timeline
Recovery from gastric sleeve surgery is generally quick due to the minimally invasive laparoscopic approach. Most patients spend one to three nights in the hospital. The immediate recovery focuses on transitioning through a liquid diet before slowly advancing to pureed foods, soft foods, and eventually regular meals over the course of several weeks. The initial rapid weight loss phase occurs in the first six months, followed by slower, steady loss as the body adjusts to the new normal.
Exploring Modern Bariatric Surgery Options
The term bariatric surgery encompasses all surgical procedures designed to treat obesity by making changes to the digestive system. While the gastric sleeve is currently the most popular choice, other options exist, and advancements are continually being made, particularly in the non-surgical space.
Endoscopic Sleeve Gastroplasty (ESG): The Non-Surgical Choice
A revolutionary, less invasive alternative to traditional surgery is the endoscopic sleeve gastroplasty, or ESG. This procedure achieves a similar effect to the surgical sleeve—reducing stomach size—but does so without external incisions. Instead, a flexible tube containing a camera and suturing device is passed through the mouth and down into the stomach. The surgeon then places sutures in the stomach lining to create a smaller, tube-shaped stomach. Because it is non-surgical, recovery time is significantly shorter, often just one or two days. While the resulting stomach restriction is usually slightly less permanent than the surgical version, ESG offers a compelling option for those who do not qualify for or do not want full surgery.
Who Qualifies for Bariatric Procedures?
Qualification for any type of bariatric surgery requires a comprehensive health evaluation. General guidelines set by leading medical organizations usually require patients to meet one of the following criteria: a Body Mass Index (BMI) of 40 or higher, or a BMI of 35 or higher accompanied by at least one significant obesity-related health condition (such as severe joint pain, hypertension, or type 2 diabetes). Regardless of the specific procedure, all candidates must demonstrate a genuine commitment to permanent lifestyle changes, including adherence to nutritional guidelines and regular physical activity.
Breaking Down the Gastric Sleeve Cost
When researching this life-changing procedure, one of the most pressing questions concerns the gastric sleeve cost. It is crucial to understand that the price tag associated with this kind of major medical intervention is not a single fixed number; it is a complex calculation that varies widely depending on numerous variables.
The cost for gastric sleeve surgery typically ranges from $10,000 to over $25,000 in the United States if paid out-of-pocket, but these figures can fluctuate drastically based on location, facility type, and included services.
Factors Affecting the Total Cost
The sticker price for a gastric sleeve surgery cost includes much more than just the time spent in the operating room. Key factors influencing the final price include:
Surgeon Fees: Highly experienced, specialized bariatric surgeons command higher fees.
Hospital or Facility Fees: This covers the operating room use, recovery room costs, and standard hospital stay (typically 1–3 nights).
Anesthesia Fees: The cost for the anesthesiologist’s time and the medications used.
Pre- and Post-Operative Care: This is often the forgotten cost. It includes required appointments with nutritionists, psychologists, and follow-up lab work, all vital for long-term success.
Insurance and Financing Options
Many patients find that their private insurance or Medicare covers the gastric sleeve if they meet specific medical criteria and complete a required pre-operative process, which often involves six months of documented diet attempts or visits with specialists. If insurance does not cover the procedure, many centers offer financing plans or medical loans. Researching specific providers and their bundled pricing structures can often help reduce the overall burden of the gastric sleeve cost.
Taking the Leap
The decision to undergo the gastric sleeve is a powerful step toward a healthier future. This procedure is a tool, providing both physical restriction and metabolic changes that make weight loss achievable and sustainable. By understanding the mechanics of gastric sleeve surgery, exploring modern alternatives like endoscopic sleeve gastroplasty, and preparing for the gastric sleeve cost, you equip yourself with the knowledge needed to make an informed choice. Consulting with an expert bariatric team is the crucial next step in beginning your transformative health journey.